Many people with diabetes and kidney problems want clear guidance on therapy choices. Evidence suggests dapagliflozin in chronic kidney disease can help protect kidney function while supporting heart health. This article translates the science into practical steps you can discuss with your care team.
Key Takeaways
- Kidney protection focus: Dapagliflozin may slow CKD progression and reduce complications.
- Evidence-based use: Large trials support benefits in both diabetes and some non-diabetic CKD.
- Know the guardrails: Start within guideline thresholds and monitor volume status and labs.
- Safety first: Watch for rare ketoacidosis, genital infections, and dehydration risks.
What Is Dapagliflozin and How It Protects Kidneys
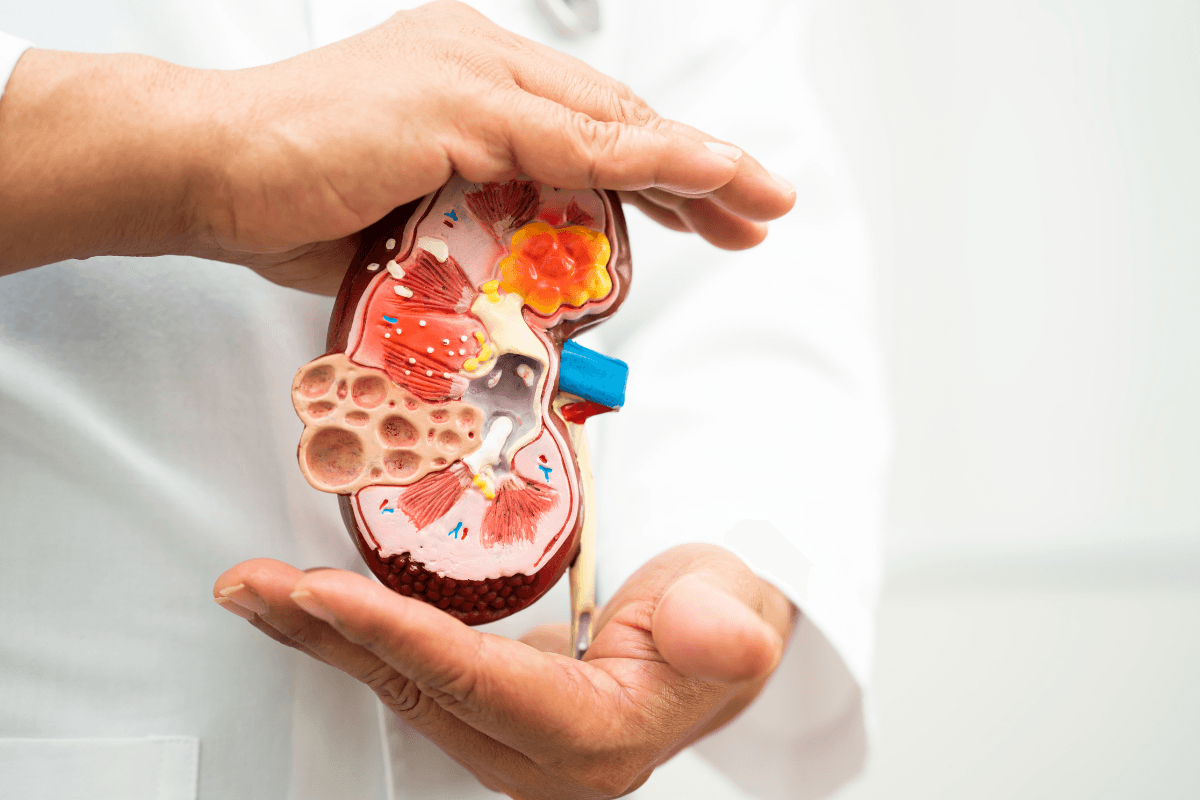
Dapagliflozin belongs to SGLT2 inhibitors, a class that increases urinary glucose excretion. By reducing sodium and glucose reabsorption in the proximal tubule, it lowers intraglomerular pressure and may slow scarring. This hemodynamic effect complements renin-angiotensin blockers and supports long-term renal health.
Regulatory labeling describes indications, contraindications, and key safety warnings for clinical decision-making. For a concise reference on approved uses and cautions, see the FDA label (this official source outlines indications and risks) FDA label. If you want a deeper dive into mechanisms, our primer provides added context; for a fuller science background, see Dapagliflozin Mechanism Overview.
People living with diabetes may also benefit from learning how this class fits into glucose care plans. For a broader look at clinical applications outside CKD, see Dapagliflozin Uses in Diabetes to understand complementary goals.
Dapagliflozin in Chronic Kidney Disease
In people with type 2 diabetes and CKD, dapagliflozin can reduce kidney stress and slow loss of filtration. Benefits extend to lowering albuminuria (protein in urine) and improving the long-term slope of eGFR (estimated glomerular filtration rate). Importantly, protective effects may also appear in certain non-diabetic CKD groups, depending on baseline kidney function and albuminuria.
High-quality evidence underpins these outcomes, including a landmark study in mixed CKD populations. For accessible trial context with outcomes and inclusion criteria, see the NEJM DAPA-CKD study (helpful for understanding who was enrolled) NEJM DAPA-CKD study. If you need a refresher on disease basics, staging, and complications, our overview of Chronic Kidney Disease summarizes progression pathways and care priorities.
Because CKD in diabetes brings unique vascular and metabolic risks, care teams integrate kidney, heart, and glucose goals together. For the diabetes-specific lens on renal injury and screening, see Diabetic Kidney Disease for timely, staged monitoring recommendations. For a broad patient-friendly introduction to therapy rationale, you can also read Promising Therapy for CKD to connect mechanisms with everyday outcomes.
Initiation Criteria and eGFR Cutoffs
Before starting therapy, clinicians check kidney function and urine protein to ensure appropriate eligibility. Many professional bodies endorse SGLT2 use across CKD stages when eGFR and albuminuria thresholds are met, and risks are managed. These parameters guide who is likely to benefit and who should wait or use alternatives.
Guidelines inform the practical guardrails used in clinics today. The KDIGO 2022 guideline offers specific thresholds and safety notes (useful when defining who to start) KDIGO 2022 guideline. When documenting “dapagliflozin eGFR cutoffs,” teams also track the urinary albumin-to-creatinine ratio to align with trial-like populations. For staging context that supports these decisions, see Stages of Diabetic Kidney Disease for risk stratification insights.
Dosing and Titration in CKD
Most adults receive a single, label-approved daily dose. In practice, clinicians emphasize steady dosing, hydration awareness, and periodic checks of renal function and electrolytes. Documented decisions align with local formularies and comorbid conditions, not solely glucose values.
Teams often note “dapagliflozin dosing in CKD” alongside a home medication review. Caution is stronger in patients on loop diuretics or with frailty, because additive fluid losses can occur. For diuretic context and practical cautions, see Lasix when reviewing overlapping dehydration risks and monitoring plans.
When to Pause and Perioperative Care
Sick days, prolonged fasting, or surgery can temporarily increase metabolic risks. Many programs use a simple pause plan to reduce complications during acute illness. The goal is risk reduction, not treatment interruption without purpose, followed by a safe and timely restart.
Clinicians often document “dapagliflozin when to hold therapy” for perioperative periods, severe dehydration, or evolving infection risks. Coordinated instructions help patients navigate temporary holds and resumption after stabilization. Labeling also highlights perioperative ketoacidosis warnings you can review (helpful for framing hold/resume steps) via the official FDA label.
Short-Term Illness and Dehydration
Illness with vomiting, poor intake, or fever can increase volume depletion and ketone production. A pre-agreed sick-day plan often includes hydration targets, glucose and ketone checks, and temporary medication adjustments under supervision. Patients should contact their care team promptly if symptoms worsen or if they cannot maintain fluids. Restart plans usually follow clinical recovery and laboratory reassessment to ensure safety. This structured approach balances renal protection with acute risk mitigation in everyday life.
Safety Profile and Monitoring
The “class effects” of SGLT2 inhibitors are well described in regulatory materials and trials. Clinicians educate about genital yeast infections, urinary symptoms, and dehydration-related dizziness. Rare events like euglycemic ketoacidosis receive focused counseling in people with high metabolic stress or restricted carbohydrate intake.
Teams explicitly discuss the “dapagliflozin risk of ketoacidosis” during illness or perioperative periods. They also watch for transient eGFR dips after initiation, usually reflecting hemodynamic shifts rather than structural injury. Monitoring often includes electrolytes, kidney function, and the urinary albumin-to-creatinine ratio to assess response. People with advanced CKD or anemia may need added checks; for background on overlapping risks, see CKD-Related Anemia to understand symptom drivers.
Clinicians also address acute kidney injury concerns in vulnerable patients, especially with diuretic changes, gastrointestinal losses, or heat exposure. Genital infection risk is reduced with good hygiene counseling and early symptom reporting. Hyperkalemia risk tends to be driven by other agents, but labs guide any needed changes. For practice alignment across systems, review the KDIGO framework again (offers practical monitoring intervals) via the KDIGO 2022 guideline.
Evidence and Outcomes
Large trials show meaningful kidney and cardiovascular benefits across a range of patients. Clinicians often summarize endpoints as slower eGFR decline, less progression to kidney failure, and fewer kidney-related events. Proteinuria typically falls, which correlates with lower long-term renal risk.
Summaries of “DAPA-CKD trial results” note consistent outcomes in key subgroups, including many with diabetes and a subset without diabetes. Improvements in the eGFR slope offer a practical way to explain long-term kidney preservation. Observational follow-up and meta-analyses reinforce these findings, though monitoring remains essential. Program leaders frequently review new data annually to refresh protocols and patient education.
Comorbid Conditions and Combination Therapy
In real-world practice, dapagliflozin is combined with blood pressure agents, statins, and glucose therapies. Teams frequently coordinate “dapagliflozin with ACE inhibitors or ARBs” to synergize albuminuria control and protect the filtration barrier. Volume status remains central, especially when other diuretics or vasodilators are added.
When choosing among SGLT2 options, comparative insights can help frame shared decisions. For a concise look at class similarities and differences, see Jardiance vs. Farxiga to understand overlapping benefits. If you are new to CKD programs or need a compact summary, our Chronic Kidney Disease page remains a useful starting point for patient education and care planning.
Recap
Dapagliflozin provides kidney and heart protection for many people with CKD, including those with type 2 diabetes. The strongest results come when therapy is started within guideline guardrails and combined with regular monitoring. Safety planning for illness and procedures helps preserve benefits while minimizing risks.
Practical programs pair clear initiation criteria with structured follow-up and education. Patients and clinicians can use the resources linked here to guide informed conversations and adapt care plans over time.
This content is for informational purposes only and is not a substitute for professional medical advice.