Key Takeaways
- Early research suggests GLP-1 medicines may influence nicotine cravings.
- These drugs are not approved as smoking-cessation treatments.
- Nicotine can worsen nausea and raise heart strain.
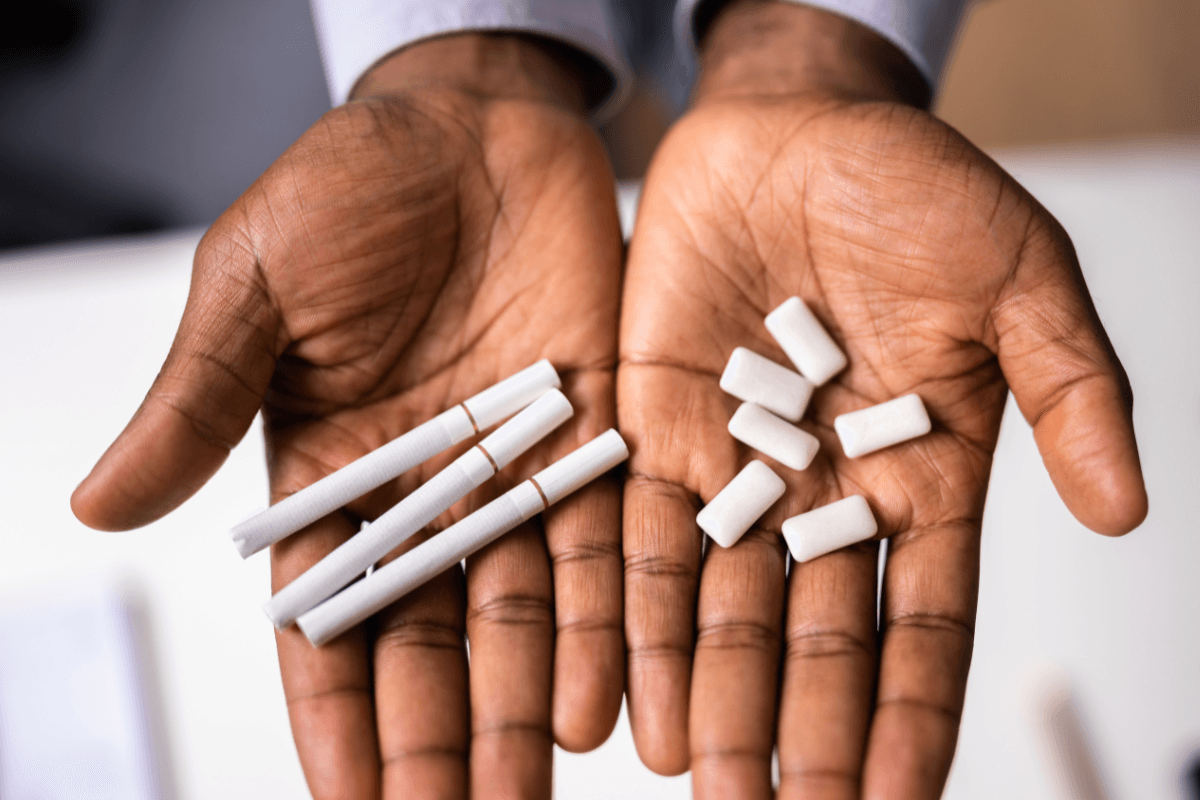
- Nicotine patches, gum, or lozenges may still be options.
- Support plus medications often works better than willpower alone.
It is common to wonder about glp 1 and nicotine together. You might be using a GLP-1 medicine for diabetes or weight management. At the same time, you may smoke, vape, or use nicotine replacement.
Why this matters is simple. Both nicotine and GLP-1 medicines affect appetite, nausea, and reward signals. Knowing what to expect can help you plan safer conversations with your clinician.
The goal here is clarity, not pressure. You will learn what research shows, what is still unknown, and which symptoms deserve a check-in.
GLP 1 and Nicotine: What Research Suggests So Far
GLP-1 receptor agonists are medicines that mimic a natural gut hormone. They are used for type 2 diabetes and, in some cases, chronic weight management. Researchers are also exploring whether they may affect substance use, including nicotine.
So far, the strongest signals come from animal studies and early human observations. Some people report fewer cravings or less “pull” toward nicotine. But these are not the same as proof, and results can vary widely.
It also helps to separate “craving changes” from “quitting.” Quitting nicotine usually involves habits, stress cues, social triggers, and withdrawal symptoms. A medication that changes appetite or reward may not fully address those pieces.
Note: Ongoing trials may clarify who benefits and how much. For a snapshot of active studies, see ClinicalTrials.gov listings in neutral, searchable form.
If you want broader reading on nicotine and other substances, browsing Addictions Topics can help you compare themes across conditions.
How GLP-1 Signals May Affect Reward, Craving, and Stress
Nicotine works partly through dopamine, a brain chemical involved in reward learning. Over time, cues like driving, coffee, or stress can trigger cravings. This is not a character flaw. It is learned biology.
Scientists are studying the GLP-1 nicotine interaction because GLP-1 receptors exist beyond the gut. They are found in brain regions tied to reward and impulse control. In preclinical models, stimulating these receptors can reduce drug-seeking behavior.
That does not mean a GLP-1 medicine “treats addiction” by itself. People can still have strong urges, especially during stress or routine triggers. Many also need targeted behavioral tools and, sometimes, established quit medications.
If you are curious how this research extends beyond nicotine, reading Reducing Opioid Addiction can provide helpful background on the same reward pathways.
Semaglutide and Nicotine: Practical Considerations
Semaglutide is the active ingredient in medicines like Ozempic and Wegovy. It can reduce appetite and slow stomach emptying. Those effects may change how “satisfying” nicotine feels for some people.
When semaglutide and nicotine overlap, the day-to-day issue is often symptoms, not efficacy. Both can contribute to nausea, heartburn, or a “queasy” feeling. If appetite drops sharply, nicotine may feel harsher on an empty stomach.
Semaglutide can also change blood sugar patterns, especially for people with diabetes. Nicotine can affect insulin sensitivity and stress hormones. That combination may matter if you use glucose-lowering medicines or have frequent lows.
For details that reflect approved indications and safety language, the FDA-approved label is a useful reference point. It helps you see what is known, and what is not addressed.
If you are comparing addiction-related research across substances, Ozempic And Alcohol Use explains why cravings may shift in some settings.
Tirzepatide and Nicotine Considerations
Tirzepatide is a dual-acting medicine (GIP/GLP-1) used for diabetes and, in some regions, weight management. Its appetite and gastrointestinal effects can be strong, especially early on. That makes symptom planning important if you also use nicotine.
With tirzepatide and nicotine, nausea and reduced appetite are common practical concerns. If nicotine is part of your morning routine, taking it without food may feel more intense. Some people also notice more reflux or stomach discomfort when both are in play.
It is also worth thinking about dehydration risk. Vomiting or reduced fluid intake can worsen dizziness and fatigue. Nicotine can sometimes mask hunger while increasing stomach irritation, which complicates the picture.
If you are comparing side-effect patterns across incretin-based medicines, Tirzepatide GI Side Effects offers context for what people report and why.
For a broader overview of one tirzepatide brand and how it differs, Zepbound For Weight Loss can help you understand the naming and indications.
Nicotine Replacement Therapy (Patch, Gum, Lozenges) While on GLP-1s
Nicotine replacement therapy (NRT) delivers nicotine without smoke. That matters because smoke exposure drives much of the long-term health risk. Still, NRT can cause side effects, and GLP-1 medicines can add to them.
One common question is whether nicotine gum and semaglutide can be used together. There is no single yes-or-no for everyone. The more useful approach is to watch for additive nausea, heartburn, hiccups, or a “too full” feeling.
Different NRT forms can feel very different on a GLP-1 medicine. Gum and lozenges may irritate the stomach if swallowed saliva builds up. Patches avoid the mouth and stomach, but they can still raise heart rate or disturb sleep in some people.
| Nicotine option | What may feel different on GLP-1 therapy | Good discussion points |
|---|---|---|
| Patch | Less stomach upset, but possible sleep issues | Timing, vivid dreams, skin irritation |
| Gum | Heartburn or nausea if swallowed | Technique, triggers, dose step-down plan |
| Lozenge | Mouth irritation, reflux in sensitive stomachs | Meal timing, nausea patterns, hydration |
| Inhaler or spray | Throat irritation, fast nicotine “hit” | Use frequency, cravings vs habits |
Tip: If nausea is the main barrier, tracking when it happens can help. Note nicotine timing, meal size, and GLP-1 injection days. Bring that pattern to your next visit for tailored adjustments.
If you are weighing prescription quit aids alongside NRT, Champix Vs Chantix can clarify naming and general differences. For a neutral look at one prescription option, see Varenicline for formulation details and standard labeling.
Some clinicians also consider bupropion as part of a quit plan. If you want to understand a common sustained-release form, Bupropion SR is a useful reference for basics and cautions.
Smoking, Vaping, and Cardiometabolic Safety While Using GLP-1 Medicines
GLP-1 and smoking intersect most clearly in heart and blood vessel risk. Smoking is a major driver of cardiovascular disease and stroke. GLP-1 medicines can improve weight, glucose, and sometimes blood pressure, but they do not erase smoking-related harm.
Vaping nicotine is different from smoking, yet it can still affect the heart and lungs. Nicotine can raise heart rate and blood pressure and can worsen anxiety for some people. If your GLP-1 medicine already causes palpitations or dizziness, it is worth mentioning nicotine use explicitly.
Also consider appetite changes during withdrawal. Many people eat more when they cut back nicotine, especially sweets. A GLP-1 medicine may blunt that effect, but it can also make it harder to meet protein and fluid needs if nausea is present.
For general quitting supports and evidence-based strategies, the CDC quitting resources summarize counseling, medications, and planning tools in plain language.
Quitting While on GLP-1 Therapy: Planning, Monitoring, and Support
Stopping nicotine can be one of the best health steps available. It can also be hard, especially if nicotine has been managing stress or attention. If you are trying to quit while on a GLP-1 medicine, planning reduces surprises.
Clinicians often watch three areas during changes: mood, sleep, and blood sugar. Irritability and low mood can be normal withdrawal symptoms, yet they still deserve support. For people with diabetes, appetite shifts and nicotine changes can affect glucose patterns.
GLP-1 therapy and tobacco use counseling can work well together because they address different pieces. The medication may help with appetite and some reward signals. Counseling targets triggers, routines, and relapse prevention, which medication cannot “teach.”
If you prefer to read about appetite-and-craving approaches beyond nicotine, Contrave And Cravings offers a helpful comparison of mechanisms and expectations.
Recap
Research is actively exploring whether GLP-1 medicines may reduce nicotine cravings for some people. The science is promising, but it is not settled. These medications are also not approved as nicotine-cessation treatments.
If you smoke, vape, or use NRT while on a GLP-1 medicine, focus on practical safety. Track nausea, hydration, mood, and glucose patterns if relevant. Bring those details to a clinician so your plan fits your body and goals.
This content is for informational purposes only and is not a substitute for professional medical advice for your personal situation.