The relationship between pancreas and diabetes shapes how your body manages glucose. When this small gland falters, blood sugar control can change, sometimes dramatically. Understanding what is happening helps you act earlier, ask better questions, and work with your care team more confidently. This guide combines clear explanations with practical, person-centered tips.
Key Takeaways
- Pancreas roles: insulin, glucagon, and digestive enzymes
- Diabetes types: type 1, type 2, and pancreatogenic (type 3c)
- Red flags: thirst, fatigue, weight loss, abdominal pain
- Care plan: screening, nutrition, meds, and monitoring
Pancreas and Diabetes: How They Interact
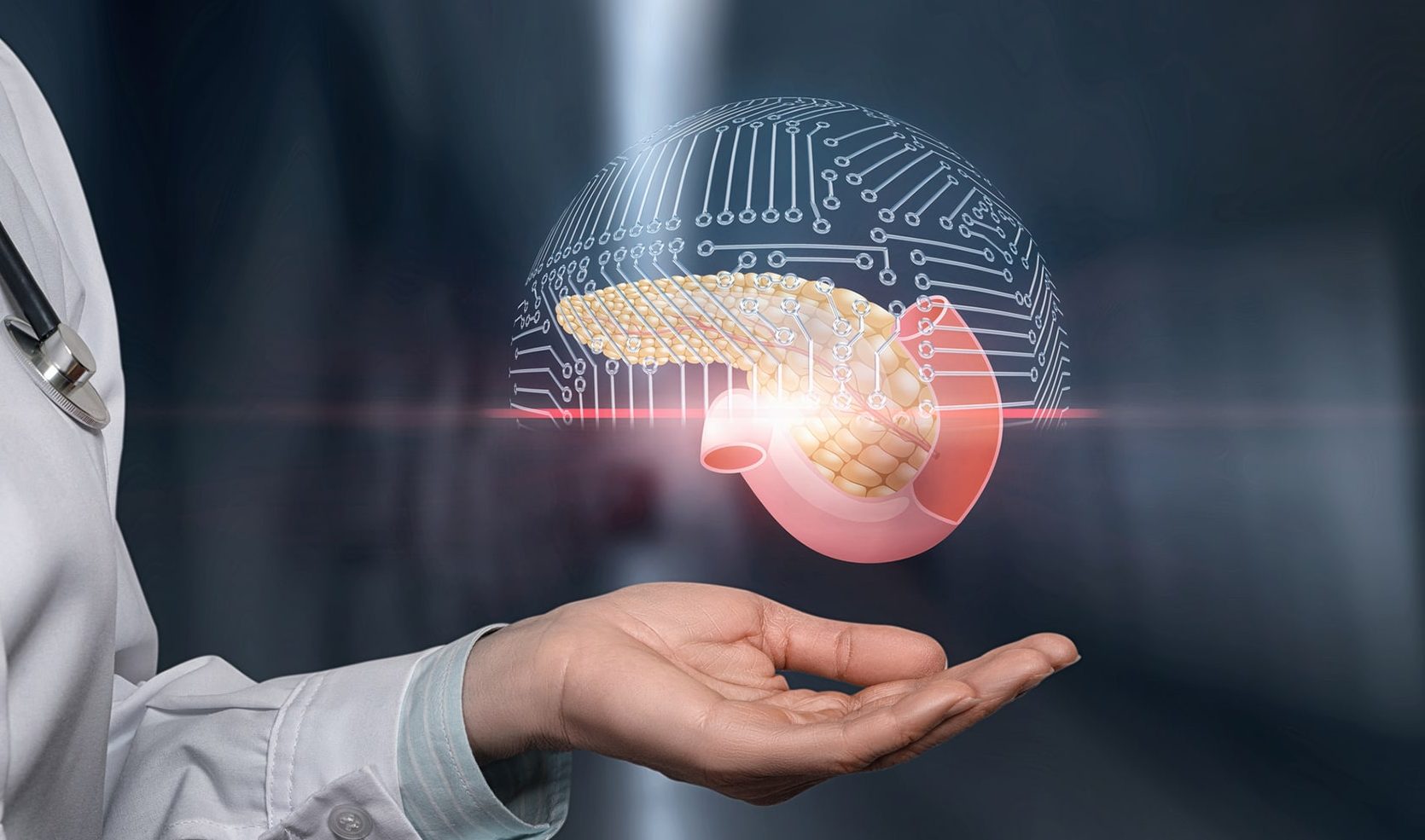
Your pancreas has two jobs. The endocrine cells make hormones, including insulin and glucagon, which balance blood sugar. The exocrine cells produce digestive enzymes that help absorb nutrients. When either system struggles, metabolism and digestion can both be affected. That is why pancreatic disorders may raise the risk of diabetes, and diabetes can worsen digestive symptoms.
In practical terms, damaged beta cells (the insulin-making cells) lead to high glucose. Over time, this can strain nerves, kidneys, and small blood vessels. If exocrine function drops, nutrient shortfalls may appear, even with a normal diet. Working with clinicians to track glucose, weight, stool patterns, and abdominal pain can surface problems early and guide safer choices.
Types of Diabetes and Core Differences
Type 1 diabetes is an autoimmune process where the immune system attacks beta cells. People usually need insulin from diagnosis. Type 2 diabetes results from insulin resistance (cells respond poorly) and a gradual drop in insulin production. Many people manage it with nutrition therapy, activity, and medications before needing insulin. A third form, pancreatogenic diabetes, occurs when pancreatic disease or surgery impairs hormone and enzyme production.
For a deeper orientation by category, see Types of Diabetes for a plain-language overview. For therapy choices and timing, our Types of Insulin guide explains onset, duration, and pairing strategies.
Recognizing Symptoms and When to Test
Thirst, frequent urination, blurry vision, and fatigue are common early signals. Unintentional weight loss and more infections may also occur. Some people notice tingling in the feet or slow-healing skin. If these worries appear, a fasting glucose or A1C test helps confirm the pattern and guide next steps.
People at risk should know the hallmark (not exhaustive) signs. Classic type 2 diabetes symptoms include increased thirst, frequent urination, and fatigue, often developing gradually. Abdominal pain, steatorrhea (greasy stools), or vitamin deficiencies can hint at pancreatic involvement. Early testing supports safer, stepwise care and lowers the odds of severe highs or lows.
What Drives Onset and Risk
Family history, aging, and visceral fat promote insulin resistance. Over time, the pancreas may not keep up with demand, and blood glucose rises. Certain medications, sleep issues, and chronic stress can add to the burden. Pancreatic disorders, including chronic pancreatitis, increase risk further by damaging both endocrine and exocrine tissue.
Several factors explain what causes type 2 diabetes, including genetics, excess adiposity, and insulin resistance. Environmental exposures may also play a role; for a research summary on metals and metabolism, see this overview of Cadmium and Diabetes for context on emerging risk science. For evidence-based screening and care principles, the American Diabetes Association updates its Standards of Care annually to reflect current consensus.
Type 3c Diabetes (Pancreatogenic) Explained
When diabetes follows pancreatic disease or surgery, clinicians may call it type 3c diabetes (pancreatogenic diabetes). Causes include chronic pancreatitis, cystic fibrosis, pancreatic cancer, and partial pancreatectomy. People can experience both insulin deficiency and digestive enzyme loss. That dual impact complicates nutrition, weight stability, and glucose targets.
Enzyme replacement can help digestion if exocrine function is low. Nutrition support often prioritizes sufficient protein and fat-soluble vitamins. For a practical look at enzyme options, see Creon Versus Other to compare formulations and dosing forms for digestive support.
How Type 3c Is Diagnosed and Distinguished
Clinicians consider the timing: Did diabetes appear after pancreatitis, pancreatic surgery, or another clear pancreatic disorder? They also look for signs of exocrine insufficiency, such as weight loss, bloating, or oily stools. Imaging, fecal elastase testing, and a history of acute or chronic pancreatitis can support the diagnosis. Glucose patterns may show a mix of fasting highs and unpredictable drops after meals, especially if digestion is impaired. The goal is to document pancreatic disease and clarify whether both hormone and enzyme deficits are present, which often changes the care plan.
Pancreatitis, Blood Sugar, and Complications
During or after inflammation of the pancreas, people may see erratic pancreatitis blood sugar levels. Acute illness can raise glucose due to stress hormones. Later, scarring can reduce insulin production. Because symptoms vary, clinicians often repeat testing over months to track stability and adjust treatment.
Long-term complications relate to both diabetes and pancreatic disease. Microvascular problems can affect the eyes, kidneys, and nerves over time. Pain, malabsorption, and weight loss may complicate daily life. A comprehensive plan addresses both sides. For enzyme questions and digestive control, our comparison Pancreaze vs. Creon offers practical distinctions patients often ask about. For public health summaries on complications, see the CDC’s diabetes overview for standard risk descriptions.
Diagnosis, Codes, and Clinical Terms
Medical records may reference “pancreatogenic” when diabetes links to pancreatic disease. In coding systems, clinicians often pair a pancreatic disease code with E13 (other specified diabetes mellitus), noting the suspected origin. Because approaches vary by country and insurer, your clinicians and billing team should determine the most accurate code set for your situation. Clear documentation of the underlying pancreatic condition usually supports better coordination.
Note: Diagnostic labels may change as evidence evolves. Ask your team to record both the pancreatic diagnosis and the diabetes type. That helps align enzyme therapy, nutrition support, and glucose targets with your health goals.
Treatment Pathways and Team Care
Care plans are individualized and often stepwise. Nutrition therapy and physical activity form the base. When medications are needed, clinicians may choose among metformin, DPP-4 inhibitors, SGLT2 inhibitors, GLP-1 receptor agonists, and basal or bolus insulin. In pancreatogenic diabetes, enzyme replacement and vitamin support can be just as important as glucose medications.
Team care may include your primary clinician, endocrinologist, dietitian, and sometimes a pain or GI specialist. Combination approaches can support stable glucose and weight. A practical medication overview is outlined in our Janumet Guide for DPP-4 plus metformin context. For sulfonylurea and meglitinide examples used in some cases, see Glimepiride and Repaglinide for class details and use-cases. If you and your clinician are weighing incretin therapy versus insulin, this comparison Ozempic vs. Insulin outlines considerations people frequently discuss.
In confirmed pancreatic origin, clinicians may tailor pancreatic diabetes treatment to include enzyme replacement, glucose agents with low hypoglycemia risk, and medical nutrition therapy. Because digestion and absorption can be inconsistent, glucose monitoring and dose adjustments may require extra caution. The ADA’s annually updated Standards of Care offer a foundation for shared decision-making.
Type 1: Special Considerations and Care
Autoimmune diabetes often presents rapidly. People may notice rapid weight loss, excessive thirst, and nausea. Diabetic ketoacidosis requires urgent care. Classic type 1 diabetes symptoms include frequent urination, fatigue, and sometimes abdominal pain or vomiting, especially near diagnosis. Families and caregivers should know the warning signs and when to seek immediate help.
Insulin education, routine ketone awareness, and flexible meal planning support daily life. Technology can help with dosing decisions and alerts. For more on insulin types and timing, this practical primer on Types of Insulin explains pairing long- and rapid-acting options. People recovering from pancreatitis or surgery may need different targets and closer follow-up, especially during weight changes or GI flares.
Living Well: Monitoring, Nutrition, and Prevention
Regular glucose monitoring, A1C checks, kidney labs, and eye exams reduce risk. Recognizing type 2 diabetes complications early allows timely interventions and referrals. Nutrition plans emphasize protein, fiber, and steady carbohydrates, with adjustments for malabsorption if present. Hydration, sleep, and stress reduction also support insulin sensitivity.
Movement helps the body use glucose more effectively. Even short walks after meals can help post-meal spikes. For remission goals and realistic expectations, see our overview Reverse Type 2 to understand what “remission” means in practice and which habits matter most. Partnering with a dietitian can translate these principles into weekly routines you can sustain.
Recap
The pancreas sits at the crossroads of blood sugar and digestion. When it falters, the body can face both glycemic swings and nutrient gaps. Clarifying your diabetes type and any pancreatic disease sharpens the care plan. Together, these details guide safer nutrition, medication choices, and monitoring.
Most people benefit from a layered approach. Start with screening and lifestyle supports, add medicines as needed, and reassess during life changes. If pancreatic disease is present, address digestion alongside glucose goals. Use trusted guidance and keep asking questions—your experience and values should shape the plan you follow.
This content is for informational purposes only and is not a substitute for professional medical advice.