Knowing your asthma triggers is the first step toward fewer flares and steadier breathing. This guide explains how irritants and allergens inflame airways, why symptoms vary, and what practical changes help day to day. You will find evidence-based tips and clear next steps you can discuss with your clinician.
Key Takeaways
- Know your trigger patterns: track exposures, symptoms, and timing.
- Use preventer medicines consistently; technique and adherence matter.
- Ventilation, cleaning, and moisture control reduce indoor exposures.
- Nighttime cough suggests uncontrolled inflammation; adjust your plan.
- Seek urgent care for severe breathlessness, lips turning blue, or silence.
Asthma Triggers: What They Are and Why They Matter
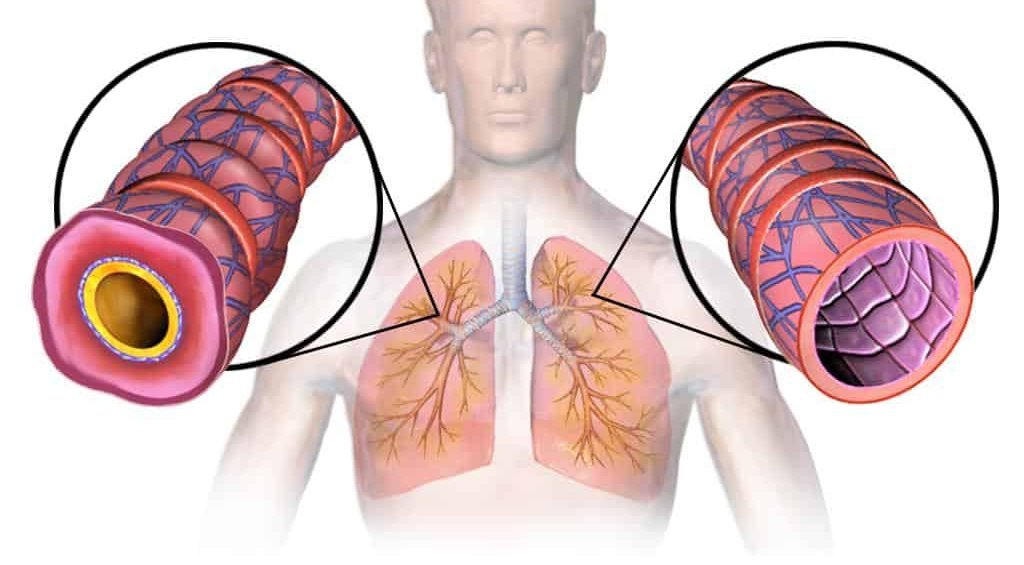
Triggers are exposures or conditions that irritate sensitive airways and prompt inflammation, mucus, and bronchoconstriction (airway tightening). They differ by person and can include allergens, respiratory viruses, smoke, air pollution, cold air, strong odors, exercise, and stress. Two people may share a diagnosis yet react to very different stimuli. That is why a personalized trigger map often works better than a generic list.
Allergic sensitization raises baseline airway reactivity, while non-allergic irritants can directly inflame the lining. Over time, frequent flares may remodel airways, making symptoms more persistent. Early identification and steady control lower those risks and help you reclaim routine activities. For practical steps on lung-health advocacy and awareness, see World Lung Day for broader prevention context.
From Irritants to Immunity: How Triggers Set Off Symptoms
In asthma, the immune system quickly responds to inhaled particles with swelling of the bronchial walls, mucus production, and smooth muscle tightening. That combination narrows the airway, causing wheeze, chest tightness, and the hallmark cough. Inflammation can persist even when you feel “okay,” which explains why flares may follow small exposures or mild colds.
Current guideline frameworks emphasize inflammation-first care with inhaled corticosteroids (ICS) and tailored add-ons. For a concise overview of recommended stepwise care, the GINA report summarizes core strategies used worldwide. For U.S.-focused practice updates, the asthma management updates outline evidence on control and safety.
Recognizing Atypical Presentations: Cough-Only Asthma
Some people mainly cough without wheeze or obvious breathlessness. This pattern is often called cough variant asthma and may be overlooked, especially in children and older adults. The cough usually worsens with exercise, laughter, cold air, or viral infections. Nighttime symptoms are common and can fragment sleep for weeks if untreated.
Diagnosis relies on a careful history plus objective tests. Spirometry (breathing test) can show reversible airflow limitation; bronchoprovocation testing can reveal hidden hyperreactivity. Your clinician may also consider reflux, vocal cord dysfunction, or chronic sinus inflammation. Keeping a symptom journal helps connect exposures to cough clusters and speeds up targeted care.
What Does an Asthma Cough Sound Like?
The asthma cough sound can be dry, tight, and repetitive, especially during viral colds, activity, or exposure to smoke or pollen. Some describe a “barking” quality, while others notice a tickle that won’t quit. During flares, coughing may alternate with wheeze or chest tightness. In advanced irritation, coughs can come in exhausting fits.
Not every harsh cough is asthma. Heartburn, postnasal drip, and certain blood pressure medicines can mimic symptoms. If you cough up discolored mucus, have fever, or notice chest pain, seek medical evaluation. Timely checks can rule out infection, consider airway imaging, or adjust your treatment plan safely. For ongoing education across lung conditions, browse our Respiratory articles for broader context on breathing health.
Stopping the Cough and Sleeping Better
When cough dominates, targeted relief and trigger control work together. Practical steps include warm fluids, humidified air when dry, short-term throat lozenges, and avoiding smoke or irritant sprays. If allergies are involved, an antihistamine may help nasal symptoms that feed the cough reflex. For allergy basics and medication considerations, see Claritin Allergy Medicine for a general overview of non-drowsy options.
Good sleep hygiene helps too: elevate your head, close bedroom windows during high pollen, and shower before bed to rinse allergens. If nighttime cough persists despite these steps, discuss how to stop asthmatic cough within your written action plan. Consider reviewing peak flow trends and recent exposures before bed to anticipate trouble and act early.
Proven Therapies and Self-Management
Most people benefit from a daily preventer plus a quick-relief inhaler. The treatment of asthma often starts with low-dose inhaled corticosteroids, which reduce airway swelling and improve control over time. Many adults also use combination therapies that add a long-acting bronchodilator for steadier symptom protection. Personalized action plans tie changes in symptoms or peak flow to clear steps you can take.
Consistent technique makes every dose count. Spacers can improve drug delivery for pressurized inhalers, and regular rinsing helps reduce throat side effects. If you use a combination ICS/LABA, your clinician may adjust dosing during viral colds or seasonal surges. For equity and access discussions around inhalers, see Inhalers For All for why device availability matters.
Controller Versus Reliever Medicines
Controllers work quietly in the background by calming airway inflammation. These include inhaled steroids and, for some, leukotriene modifiers or biologics. Relievers act fast on airway muscles to ease tightness during symptoms. Many action plans now prefer reliever strategies that also include an anti-inflammatory component, which may lower severe flare risk compared with short-acting bronchodilators alone. If you use a combination device, your care plan might allow extra doses during early flare signs, but only as instructed. Medication choices are individualized, balancing benefits, side effects, and personal goals.
For readers comparing device options, Wixela illustrates a common combination inhaler; review it alongside your clinician’s guidance to match therapy with symptoms. For additional community initiatives around breathing care, see Respiratory Care Week for perspectives on care teams and support.
Prevention Strategies That Reduce Flares
Prevention starts with routine controller use, updated vaccinations, and a simple plan you can follow under stress. Track patterns across seasons and activities, and tighten controls before high-risk periods. If exercise triggers symptoms, a warm-up and proper pre-activity medicine can help. People with allergic patterns may also benefit from dust-mite covers, regular hot washing of bedding, and reducing soft surfaces where allergens linger.
Cleaner indoor air pays off. Vent patchy areas like bathrooms and kitchens, avoid indoor smoking and burning candles, and consider HEPA filtration if outdoor pollution or wildfire smoke drifts indoors. Discuss how to prevent asthma attacks in your action plan and rehearse steps with family. For broader allergy-immune learning, explore Allergy Immunology articles to connect environmental control with symptom relief.
When Medicines Aren’t Working: Troubleshooting and Red Flags
Sometimes symptoms linger despite therapy. If you notice an asthma inhaler not helping cough, check technique first and confirm the device’s dose counter. Consider recent viral infections, allergen surges, or new exposures at work or home. Reflux, sinus disease, and vocal cord dysfunction can mimic or worsen asthma, so bring up any throat tightness, heartburn, or hoarseness.
Serious signs include struggling to speak, ribs pulling in with breaths, blue lips, or a quiet chest with minimal air movement. Those are medical emergencies—seek immediate care. Afterward, plan a follow-up to reassess triggers, update tests like spirometry, and review step-up options. For community awareness and prevention themes, World Lung Day offers context on reducing risks across environments.
Home and Food Triggers You Can Change
Indoor air typically carries dust mites, pet dander, molds, cleaning fumes, and cooking particles. Focus on what you can modify: encase mattresses, wash bedding weekly in hot water, run bathroom fans, and fix leaks quickly. Choose fragrance-free cleaners and rinse mops thoroughly. If outdoor pollution is high, close windows and run a HEPA purifier where you spend most time.
Food rarely triggers classic asthma, but it can worsen reflux or postnasal drip, which aggravate cough and throat irritation. Large late meals, alcohol, and very spicy dishes may be culprits for some people. Keep a brief log during symptom spikes; patterns often emerge within days. For general allergy sleep-aid considerations, review Diphenhydramine XST Allergy for context on sedating antihistamines—then discuss suitability with your clinician.
Tests, Monitoring, and Action Plans
Diagnosis and control checks rely on objective data. Spirometry and bronchodilator response testing can document reversible obstruction. When baseline tests are normal, bronchoprovocation may reveal hidden hyperreactivity. Peak flow meters offer a simple, daily gauge of airway status at home. Tracking morning and evening readings helps flag early dips, sometimes days before symptoms worsen.
Written action plans translate those signals into steps. Color-zone formats map symptoms and peak flow ranges to matching actions. Bring your plan to every visit and update it after flares or life changes. For more background on triggers and exposures, the CDC overview on common triggers provides practical examples across settings.
Recap
Asthma control improves when you know your patterns, use preventers consistently, and make targeted changes at home and work. Pair those steps with regular check-ins and an action plan you actually use. Small daily choices compound into steadier breathing and fewer surprises.
Tip: Keep a two-week trigger and symptom diary. Bring it to your next visit to speed up personalized adjustments that fit your life.
For more lung-health stories and resources, explore our Respiratory coverage and browse related Respiratory products for device education and comparisons.
This content is for informational purposes only and is not a substitute for professional medical advice.