Many people first learn about kidneys after a lab test flags concern. Understanding what is chronic kidney disease early helps you ask focused questions and plan care with your clinical team.
Key Takeaways
- Early detection matters: small changes in labs can guide prevention.
- Stages use eGFR and urine albumin to classify kidney damage.
- Symptoms are subtle; fatigue, swelling, and sleep changes are common.
- Diet, blood pressure control, and medicines can slow decline.
- Dialysis and transplant restore function when kidneys can’t meet needs.
What Is Chronic Kidney Disease
Chronic kidney disease (CKD) describes lasting kidney damage or reduced kidney function over three months or longer. Clinicians monitor kidney filtration using estimated glomerular filtration rate (eGFR) and assess injury with urine albumin. Together, these measures help stage disease, guide treatment, and track risk.
CKD often develops from long-standing conditions like diabetes and hypertension. It can also stem from autoimmune disease, inherited disorders, recurrent kidney stones, or prolonged medication toxicity. For a clear primer on definitions and causes, see the NIDDK overview from the National Institutes of Health, which explains CKD progression and testing in accessible terms.
To explore CKD basics on our site, this summary of Chronic Kidney Disease offers definitions and causes you can reference during appointments.
Understanding CKD Stages, eGFR, and Albuminuria
Clinicians group chronic kidney disease stages by eGFR and urine albumin levels. eGFR estimates the kidneys’ filtering capacity; albumin in urine signals damage to the filtration barrier. Staging clarifies risk of complications and the need for targeted interventions. You may see eGFR levels by CKD stage listed from G1 (normal/high) to G5 (kidney failure), while albuminuria categories range from A1 (normal to mildly increased) to A3 (severely increased).
Why this matters: the combination of G and A categories estimates future risk and guides monitoring intervals, medication choices, and referrals. For current staging and care recommendations, the KDIGO clinical practice guideline summarizes risk-based strategies for slowing CKD and preventing complications; review the latest clinical practice guideline as a reference for shared decision-making. For comparisons with diabetes-related stages, see 5 Stages of Diabetic Kidney Disease for context on overlapping risks.
Recognizing Symptoms and Common Complications
Many people have few or no chronic kidney disease symptoms at first. Over time, fatigue, leg swelling, itchy skin, sleep disturbance, and difficulty concentrating can appear. Muscle cramps, appetite loss, and changes in urination patterns also occur. These signs can be subtle, so regular labs and blood pressure checks remain essential.
Complications may include anemia, bone and mineral disorders, metabolic acidosis, and cardiovascular disease. Anemia often presents with low energy and shortness of breath. If anemia is a concern in your plan, see our overview of Chronic Kidney Disease Related Anemia for causes and treatment pathways you can discuss with your clinician.
Women’s Kidney Health: Sex-Specific Risks and Signs
Clinicians recognize that kidney disease symptoms in females can present differently across life stages. Heavy periods may worsen anemia; urinary infections can be more frequent; and pregnancy introduces unique blood pressure and proteinuria considerations. Many women also shoulder caregiving responsibilities, delaying care or missing follow-ups.
It helps to watch for swelling in the feet, frothy urine, persistent fatigue, and elevated home blood pressure readings. If urinary pain or flank discomfort recurs, evaluating for stones is reasonable; see Kidney Stones for background on symptoms and when imaging is considered, especially if infections repeat.
How CKD Is Diagnosed and Monitored
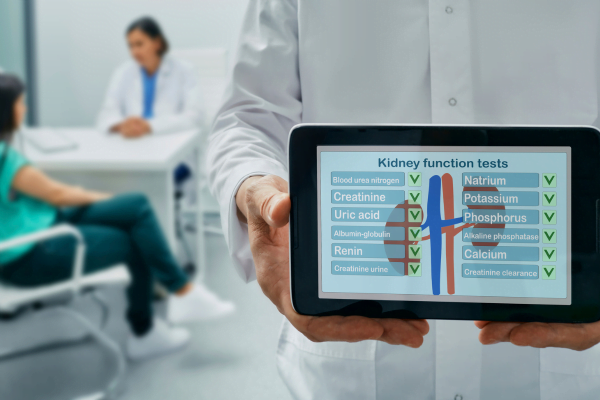
Diagnosis starts with blood and urine testing over time. Creatinine-based eGFR estimates filtering ability, while urine albumin-to-creatinine ratio (uACR) evaluates kidney injury. Persistent abnormalities over three months generally confirm chronic disease rather than a short-term problem. Your clinician may add imaging or serologic tests if autoimmune, obstructive, or hereditary causes are suspected.
Key Tests Explained
eGFR can fluctuate with hydration, diet, and muscle mass, so trends matter more than a single value. Creatinine and cystatin C may be combined for better accuracy in some cases. The uACR helps quantify albuminuria and guide therapy intensity. Additional labs monitor electrolytes, acid-base balance, bone-mineral markers, and anemia. When interpretation is complex, a nephrology referral supports a comprehensive plan. Discuss timing and frequency to align lab monitoring with your risk and goals.
Structured testing supports chronic kidney disease diagnosis and clarifies complication risks. Keep copies of your results, medications, and blood pressure readings to spot patterns between visits.
Managing CKD Before Kidney Failure
The foundation of kidney disease treatment is risk reduction: manage blood pressure, optimize diabetes care, treat albuminuria, and adopt a kidney-friendly diet. Sodium restriction can reduce fluid retention; tailored protein intake may lower uremic toxin burden; and adequate calories help maintain muscle. Regular activity, sleep, and tobacco cessation add incremental protection.
Medication choices depend on your stage, albuminuria, and comorbidities. ACE inhibitors or ARBs often reduce proteinuria and protect the filtration barrier. SGLT2 inhibitors may lower progression risk in appropriate patients with or without diabetes. For a deeper look at SGLT2 therapy, see Dapagliflozin Therapy for mechanisms and study highlights. To understand an ACE option used for blood pressure in CKD care, review Lisinopril 10 Mg Tablet for safety considerations to discuss with your clinician.
Stage 3b: Focused Care and Follow-Up
People labeled with chronic kidney disease stage 3b often need closer monitoring for anemia, mineral-bone disorders, and cardiovascular risks. eGFR usually ranges approximately 30–44 mL/min/1.73 m², and albuminuria level influences risk. This is a key time to review medicines, vaccine status, diet, and referral needs. You and your care team can set goals around blood pressure, glucose targets, and symptom tracking.
Therapy may include renin-angiotensin system blockers, SGLT2 inhibitors, and agents addressing acidosis, phosphorus, or potassium in selected cases. If you live with diabetes, see Diabetic Kidney Disease for context on glucose management and kidney protection. For recent data connecting diabetes therapy and CKD pathways, this explainer highlights effects worth discussing at your next visit: The Impact of Dapagliflozin on CKD in Diabetes.
Symptoms, Daily Life, and Support
Day-to-day living with CKD requires practical adjustments. Plan meals that balance protein, fiber, and potassium while fitting your stage and preferences. Track weight trends and swelling so you can flag fluid shifts early. Sleep hygiene and gentle exercise often help energy, mood, and blood pressure.
Discuss work schedules, caregiving duties, and travel plans with your care team. Small strategies—medication organizers, blood pressure logs, and shared calendars—make complex regimens manageable. When symptoms like itch, cramps, or taste changes escalate, report them quickly; these clues often precede lab shifts and allow timely changes in therapy.
Medications, Diet, and Prevention Strategies
As disease progresses, clinicians often review chronic kidney disease medication lists for kidney safety. Some pain relievers and contrast dyes can stress the kidneys, while dose adjustments may be needed for antibiotics, diabetes drugs, and blood thinners. Your pharmacist can help reconcile prescriptions and supplements to reduce interactions.
Nutritional counseling can align protein intake with your stage and symptoms. People with high phosphorus may need binders; if levels are difficult to control, ask about options like Velphoro for background on phosphate binding in CKD. If potassium runs high, diet changes and binders may help; see Lokelma to understand how hyperkalemia is managed and what questions to bring to visits. Prevention centers on blood pressure control, healthy weight, and not smoking. Vaccinations, especially for flu and pneumonia, can reduce hospitalizations and preserve stability.
Dialysis and Kidney Transplantation
When kidneys can no longer support health, renal replacement therapy maintains life and quality. Dialysis removes toxins and fluid through hemodialysis in a center or at home, or through peritoneal dialysis using the abdominal lining. Modality choice depends on lifestyle, other medical conditions, access placement, and personal goals. Transplantation can offer greater freedom and better long-term survival compared with dialysis for many candidates.
Before starting therapy, clinicians discuss risks, benefits, and supportive care. Planning early enables access creation, transplant evaluation, and shared decision-making based on values. For an accessible overview of treatment choices, the NIDDK provides a balanced dialysis and transplant summary; review this treatment overview to prepare questions. To understand post-transplant risks and monitoring, see Kidney Transplant Rejection for signs and follow-up routines.
Related Conditions and Cardiometabolic Risk
CKD seldom occurs alone. High blood pressure, heart disease, and diabetes intertwine with kidney health and accelerate damage. Statin therapy and antiplatelet strategies may be considered to reduce cardiovascular events, while glucose-lowering treatments with kidney benefits are increasingly prioritized in care plans. Coordinating care between primary, nephrology, cardiology, and endocrinology teams helps align goals and simplify regimens.
If you want to explore kidney–heart–diabetes overlap therapies, this primer on Jardiance for Heart Failure explains cardiorenal concepts you can discuss with your clinicians. Realistic risk reduction often combines lifestyle, medication, and close monitoring rather than a single intervention.
Recap
CKD care begins with awareness, continues with monitoring, and advances through tailored treatment. Clear staging, symptom tracking, and prevention keep options open longer. When kidney function declines, dialysis and transplant can restore balance and stability. Keep asking questions, bring your data to visits, and revisit decisions as your goals evolve.
Note: This content is for informational purposes only and is not a substitute for professional medical advice.