Key Takeaways
- Follow combivent respimat instructions to prime, inhale, and store safely.
- Use the device as directed for COPD maintenance, not asthma relief.
- Check technique regularly; small fixes can improve symptom control.
- Watch for side effects and interactions; report concerns promptly.
Using your inhaler correctly can feel overwhelming at first. This guide breaks down technique, dosing, and safety in clear steps. We pair clinical terms with plain language so you can understand the why behind each step. With careful practice, you can reduce errors, breathe easier, and feel more confident.
Combivent Respimat Instructions
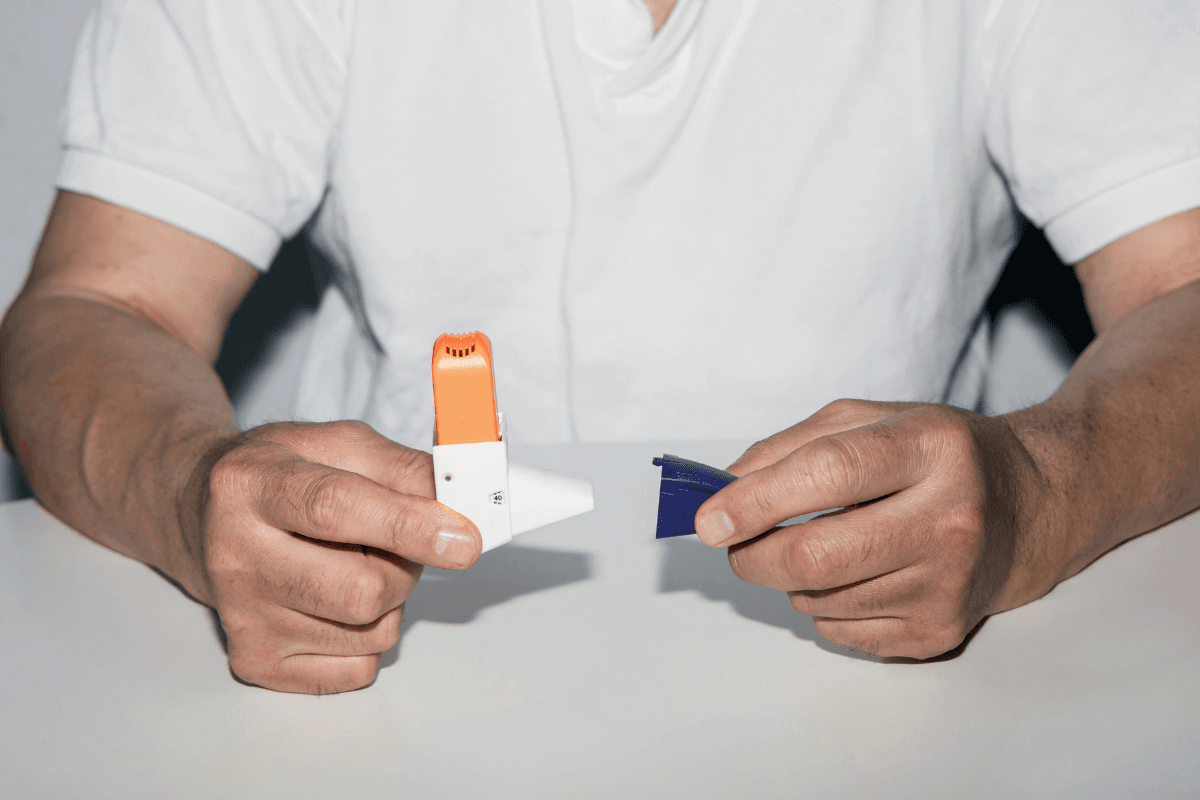
Start by preparing the cartridge and inhaler body. Insert the cartridge fully into the inhaler base until it clicks, then twist firmly to seat it. Keep the cap closed while loading. To prime a new or unused device, point it away from your face and press the dose-release button until a visible mist appears, then repeat three more times.
For daily use, hold the inhaler upright with the cap closed. Turn the base until it clicks. Open the cap, sit or stand upright, and breathe out gently, away from the mouthpiece. Seal lips around the mouthpiece without covering the vents. Start a slow, deep breath and press the button once, continuing to inhale fully. Hold your breath for up to ten seconds, then breathe out slowly. Close the cap. If a second puff is prescribed, repeat all steps from loading the base.
Tip: Clean the mouthpiece weekly with a slightly damp cloth. Wipe the dose indicator window so you can track remaining puffs.
Dosage Basics and Indications
This medicine combines ipratropium bromide (anticholinergic bronchodilator) and albuterol sulfate (beta2-agonist bronchodilator). Together, they help open constricted airways in chronic obstructive pulmonary disease (COPD). Clinicians may consider the device for maintenance and relief of bronchospasm in COPD, based on individual needs and response. Always follow your clinician’s directions for dosing frequency and timing.
Discuss the Optimal Combivent Dosage for context on typical schedules and adjustments. The phrase combivent respimat dosage refers to how often puffs are taken each day. Dose limits exist to reduce adverse effects, including tremor or palpitations. For authoritative background on indication and use, see the official prescribing information published by regulators.
Technique Checks and Common Errors
Patients often inhale too fast, press the button too late, or miss the breath-hold. These errors reduce lung deposition and waste medicine. Schedule a technique check with your clinician or pharmacist, especially after symptoms change or a new device is started. Short, hands-on coaching can improve outcomes.
Keep a checklist: prepare the dose, exhale away, seal well, press at the start of a slow breath, then hold. If your clinician recommends a spacer or chamber for coordination issues, ask whether it suits a soft-mist device. Mention your experience using a combivent inhaler so the coach can tailor tips. For a practical walk-through, see Mastering Combivent Respimat for a step-by-step walkthrough.
Nebulizer vs Respimat: When and How
Some patients use nebulized ipratropium/albuterol during exacerbations or when they cannot coordinate inhalation. Nebulizers deliver medication over several minutes via mask or mouthpiece. The soft-mist inhaler is portable and precise, but it requires correct timing and breath technique. Your clinician may prefer one method depending on symptoms, dexterity, or access.
Clarify dosing differences rather than assuming equivalence between devices. Ask how your nebulized dose relates to inhaler puffs you take daily. If you use a home nebulizer, document frequency and symptom response. The phrase combivent nebulizer may appear in your plan when nebulized therapy is considered. For dose comparisons and maintenance planning, see Combivent Dosage Overview for dosage nuances and context.
Mechanism, Classification, and Rescue Role
This combination acts via two pathways. Ipratropium reduces cholinergic tone in the airways, while albuterol relaxes airway smooth muscle through beta2 receptors. The complementary mechanism can improve airflow and reduce dynamic hyperinflation in COPD. Each ingredient has a short onset, which helps relieve bronchospasm when used as directed for COPD.
Patients often ask about rescue roles. The phrase is combivent a rescue inhaler means whether to rely on it for sudden symptoms. Follow your clinician’s plan; some patients carry a separate quick-relief inhaler. For management principles, the GOLD COPD guidelines provide neutral, evidence-based recommendations to discuss at your next visit.
Safety Flags, Contraindications, and Heart Rate
Tell your clinician about glaucoma, urinary retention, prostate issues, cardiovascular disease, or arrhythmias. These conditions can influence safety. Beta-agonists may raise heart rate or cause tremor, while anticholinergics can worsen narrow-angle glaucoma. Monitor new or worsening symptoms and report sustained palpitations, chest pain, or vision changes promptly.
Know your combivent contraindications as listed in official labeling and discuss them before starting therapy. Provide a complete medication list, including over-the-counter decongestants or herbal stimulants. If you experience persistent tachycardia or dizziness after use, stop and seek medical advice. For an accessible overview of benefits and risks, see the MedlinePlus overview prepared for patients and caregivers.
Comparing to Spiriva: Devices and First-Time Use
Many COPD regimens also include a long-acting muscarinic antagonist, such as tiotropium. Device technique matters across brands. If your plan includes tiotropium soft-mist, review how to use spiriva respimat with your clinician to reduce errors. First-time priming and daily steps differ slightly, so confirm timing and breath-hold rules.
Some patients previously used capsules with a puncture device. If you are switching from a capsule device, ask for hands-on training and a spacer discussion if coordination is difficult. For related comparisons of controller medicines, see Advair Dosage Forms for a broader perspective on inhaled therapies. If you’re deciding between devices, Reducing Asthma Attacks offers prevention principles that also inform technique goals.
Pairing With Albuterol and Other Bronchodilators
Patients sometimes use a short-acting beta-agonist for quick relief. Ask your clinician about spacing between products and signs of overuse. The question can you take combivent and albuterol together should be answered within your personalized action plan. Overlapping beta-agonists may increase side effects, including tremor and palpitations.
Keep a symptom diary that records triggers, rescue use, and recovery times. Share this record during follow-up visits to fine-tune your regimen. For a broader look at medication combinations and when adjustments make sense, see Side Effects Explained to understand warning signs that warrant review.
Directions and Reliable Support Resources
When you need official directions, rely on manufacturer-provided materials and clinical guidance. The phrase combivent respimat package insert refers to the full labeling document with safety and use information. Bookmark a trusted source for updates, as device instructions or safety notices can change. Keep a printed copy in your medication folder.
For a concise refresher on daily use, see Mastering Combivent Respimat for a step-by-step walkthrough before your next technique check. If you’re confirming dose timing, consult Optimal Combivent Dosage for detailed rationale to discuss with your clinician. To compare alternatives and delivery systems, Combivent Dosage Overview provides helpful context on scheduling and monitoring.
Practical Troubleshooting and Maintenance
If the spray becomes weak or irregular, confirm the dose indicator shows remaining puffs. Re-prime the device if not used for several weeks, following the initial steps but fewer sprays, as directed by labeling. Check that the cartridge is seated, the air vents are clear, and the mouthpiece is clean. Replace the inhaler once the indicator reaches zero, even if it still sprays.
Store the inhaler at room temperature, away from excess heat and moisture. Keep the cap closed between uses to protect from dust. Do not freeze the device. For patients comparing brands or considering device availability, the Combivent Respimat Inhaler page lists strengths and components so you can verify the product name. If your regimen includes tiotropium, review the Spiriva Respimat Inhaler listing to understand device differences before training.
When to Reassess: Symptoms, Side Effects, and Adherence
Bring your inhaler to every appointment for a quick demonstration. Report any change in breathlessness, nighttime symptoms, or activity tolerance. Frequent rescue use, repeated exacerbations, or bothersome side effects suggest that your plan needs review. Document missed doses, technique issues, or financial barriers that affect adherence.
Plan a structured technique review after hospitalizations or major medication changes. Ask about peak flow tracking or symptom questionnaires to quantify progress. If overlapping therapies complicate your schedule, a simplified plan may help. For safety-focused reading, see Combivent Side Effects to learn which symptoms deserve prompt attention and why they matter.
Recap
Correct technique, consistent dosing, and vigilant safety checks can improve your day-to-day breathing. With small adjustments and regular coaching, this inhaler can fit smoothly into your COPD plan. Keep learning, keep practicing, and keep asking questions during every visit.
Note: For additional background, the neutral prescribing information and the concise MedlinePlus overview are reliable starting points outside clinic hours.
Medical disclaimer: This content is for informational purposes only and is not a substitute for professional medical advice.