For people using mealtime insulin, understanding options reduces daily stress. If you have wondered what is short acting insulin, you are not alone. This class helps cover food-related glucose rises quickly. Clear guidance empowers safer choices and steadier days.
Key Takeaways
- Mealtime coverage: Works around eating to limit post-meal spikes.
- Regular insulin: The classic short-acting option used for decades.
- Pairing matters: Often combined with basal (background) insulin.
- Safety first: Watch for low blood sugar and carry carbs.
- Plan ahead: Timing, dosing, and site care support steadier control.
What Is Short Acting Insulin
Short-acting insulin is designed to manage blood glucose around meals. Clinicians often use it to cover carbohydrate intake or correct higher readings. In practice, this class begins working relatively soon and may last several hours. It helps narrow the spike between eating and your body’s response.
Regular human insulin is the standard short-acting type. It can be given subcutaneous (under-the-skin) before meals and, in some settings, may be used by protocols in clinics or hospitals. For a broader clinical overview, the American Diabetes Association provides insulin therapy guidance that explains roles and safety across regimens insulin therapy guidance. Your care team decides the right approach based on your history and daily patterns.
How It Works and When It’s Used
Short-acting insulin helps your body move glucose into cells after eating. It also supports correction of unexpectedly high readings between meals. You might use it in a fixed meal plan or an insulin-to-carbohydrate approach. Your prescriber will tailor the strategy to match your lifestyle and goals.
Clinicians may adjust dose timing around food, activity, and recent glucose trends. In hospitals, regular insulin may be used under supervision in special circumstances. For labeled indications, administration routes, and safety details, see this MedlinePlus overview of regular insulin medication details. These principles matter because consistent timing can reduce swings and support predictable days.
Examples and Names: Mealtime Options
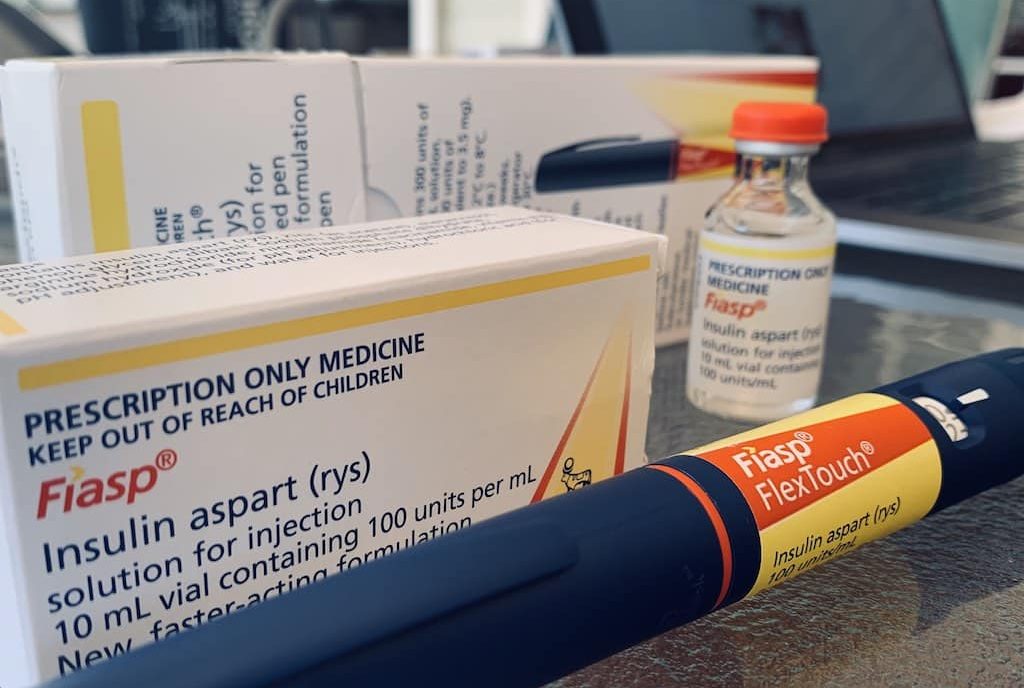
Many people first learn that short-acting insulin examples include regular human insulin, such as Humulin R and Novolin R. These are time-tested options used before meals and as correction doses. Some people also discuss faster analogs for comparison, which are in a different class.
If you are comparing very fast choices, see this primer on Rapid Acting Insulin for very fast mealtime options. To explore typical onset and peak patterns of a rapid analog, review Lispro Insulin Peak to compare onset and peak. For a concrete analog example, this Novorapid Cartridge listing helps illustrate formulation forms and use contexts.
NPH and Regular: How They Work Together
In many regimens, nph insulin and regular insulin appear together. Regular insulin addresses meals and corrections, while NPH (Neutral Protamine Hagedorn) provides intermediate background coverage. This pairing can support steady control when matched to your eating schedule and activity level. Premixed products sometimes combine these actions for simplicity.
Understanding where NPH fits helps you plan mornings, evenings, and snacks. For timing characteristics and basal roles, visit Intermediate Acting Insulin for NPH basics and timing. When selecting a broader framework, also scan Different Insulin Types for a cross-category comparison that highlights daily use cases.
Administration and Patient Teaching
Safe practice starts with regular insulin medication administration education. People are usually taught subcutaneous injections in the abdomen, thigh, or upper arm. Rotating sites helps limit lipohypertrophy (fatty tissue changes) and promotes steadier absorption. Your team may suggest tracking sites in a simple log.
Give yourself time to prepare before meals, and build routines that fit your day. Wash hands, check your glucose, and align your dose with food plans. Needle comfort and technique can improve adherence; for needle sizing and comfort notes, see BD Nano Pro Pen Needles Ultrafine. If you want a broader overview of categories, the Five Types Of Insulin is helpful for a quick taxonomy summary.
Safety and Side Effects
Common short-acting insulin side effects include low blood sugar, injection site redness, and occasional swelling. Hypoglycemia (low blood sugar) can cause shakiness, sweating, or confusion. Carry fast carbohydrates, and learn how your symptoms present. Keep friends or family informed about severe signs and when to seek help.
Allergic reactions are uncommon but possible. If you notice widespread rash, swelling, or trouble breathing, medical care is urgent. For practical prevention strategies, the CDC provides hypoglycemia safety tips suitable for everyday planning hypoglycemia safety tips. These habits matter because preparedness helps you correct lows calmly and safely.
Basal Context and Duration
Short-acting insulin targets meals; basal insulin keeps background levels steadier between meals and overnight. People often combine these in a basal-bolus plan. When evaluating basal choices, it helps to compare long-acting insulin duration, onset consistency, and daily rhythm. This makes it easier to align your schedule and your treatment.
For basal options overview, see Long Acting Insulin for basal options overview. You can also review Different Insulin Types to connect mealtime and background roles. If you want additional context on faster mealside agents, revisit Rapid Acting Insulin for very fast mealtime options.
Tools, Charts, and Costs
Planning tools reduce guesswork and support consistency. Clinicians may share printed guides or digital trackers for doses, meals, and readings. People also learn from visual overviews that compare action profiles across the day. A well-labeled chart can improve memory and strengthen self-management routines.
Access and affordability matter as much as technique. If you are navigating nph insulin cost, ask your team about assistance resources and coverage options. For structured comparisons, see Five Types Of Insulin for a quick taxonomy summary and links to related topics. For broader education across conditions, browse our Diabetes Articles to find practical education beyond medications.
Recap
Short-acting insulin supports meals and corrections, while basal insulin maintains background stability. Regular human insulin is the foundational short-acting choice. You can pair it with NPH, long-acting, or other components, depending on your regimen. The goal is a predictable pattern that fits your meals, activity, and preferences.
Success comes from small, repeatable steps. Build a routine for injection prep, glucose checks, and symptom awareness. Use checklists, site rotation logs, and simple notes about meals. When questions arise, bring them to your clinician. With steady practice and clear communication, most people can reduce swings and lighten the daily burden.
Tip: Keep a compact “pre-meal” checklist in your phone notes to support timing, site rotation, and readiness to treat lows.
This content is for informational purposes only and is not a substitute for professional medical advice.