Knowing when insulin rises to its strongest effect helps you plan meals and avoid lows. Understanding the lispro insulin peak can also reduce stress and support steadier days. This guide translates clinical timing into clear, everyday steps you can use. It balances safety details with practical planning tips.
We walk through rapid-acting, short-acting, intermediate, and long-acting profiles. You will see how onset, peak, and duration vary across types, and why that matters for meals, activity, and overnight coverage. We also include a quick reference chart and reliable sources for deeper reading.
Key Takeaways
- Peak matters most: match meal timing to action.
- Lispro rises quickly, then fades within several hours.
- Regular insulin peaks later than rapid analogs.
- NPH has a wide peak window; watch for overnight lows.
- Glargine is near “peakless”; it supports basal coverage.
Understanding the Lispro Insulin Peak
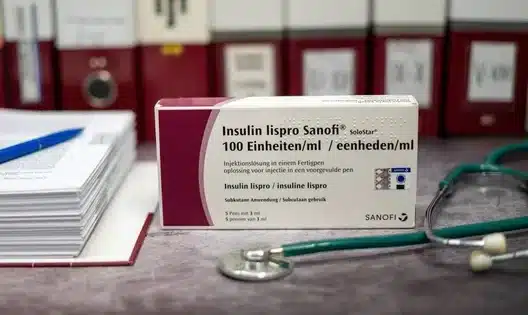
Insulin lispro is a rapid-acting analog designed for mealtime coverage. After subcutaneous injection, its action builds swiftly, then declines over several hours. The peak reflects the period when blood glucose–lowering effect is strongest. Your own peak can shift with dose, site, temperature, and activity level.
Clinical references note that many people see the strongest effect about one hour after dosing, with a total effect window of roughly three to five hours. Always consider individual variability and your care plan. For label-based details on pharmacodynamics and safety, review the Humalog prescribing information from the U.S. FDA (official product labeling), which summarizes timing ranges and hypoglycemia risks.
Onset and Duration of Rapid-Acting Insulins
Rapid-acting insulins, including lispro, aspart, and glulisine, are designed to cover meals and correction doses. Typical onset is within minutes; many people experience meaningful activity around 10–20 minutes after injection. When discussing lispro onset of action, clinicians often emphasize that absorption speed is sensitive to injection site, recent exercise, and local blood flow.
Most rapid-acting analogs reach strong activity about an hour after administration and tail off by three to five hours. Precision matters less than consistency: choose similar injection sites at similar times when possible. For a plain-language overview of how these agents work, see Rapid-Acting Insulin for context and comparisons (What Is Rapid-Acting Insulin), which explains use around meals and corrections.
Regular Insulin: How It Compares
Compared with lispro, regular insulin has a slower rise and a later peak. Many patients notice the regular insulin peak between two and four hours after dosing. Because of this delay, some care plans schedule regular insulin further ahead of meals to better match digestion. That timing decision belongs to you and your prescriber.
Regular insulin often remains active for five to eight hours, which can overlap with the next meal. That longer tail raises the risk of stacking if doses are taken too close together. For more background on brand differences among mealtime options, see Humalog vs. Novolog for mechanism highlights and substitution considerations (Humalog vs. Novolog). Label-based data for regular insulin appear in FDA-approved references (Humulin R prescribing information), which outlines onset, peak, and duration.
Intermediate-Acting (NPH) Basics
NPH stands for Neutral Protamine Hagedorn, an older basal insulin that remains widely used. It has a delayed rise and a broad, variable peak. Many people observe the nph insulin peak between four and twelve hours after injection. That range depends on dose size, timing (morning versus bedtime), and whether it is combined with short-acting insulin.
This broad peak can increase overnight low risk, especially with evening doses. If a dose is taken around 8:00 a.m., many users notice stronger activity late morning through afternoon. That effect can interact with lunch or activity; planning snacks and checking glucose may help. For context across insulin families, see Types of Insulin for plain-language descriptions and common use-cases (Types of Insulin).
Long-Acting Basal Insulins
Long-acting insulins, like insulin glargine and detemir, are built for steady background coverage. They are often described as “peakless,” though some people still notice mild variations. When people ask about lantus peak time, many clinicians explain that glargine shows a relatively flat profile across 20–24 hours. Individual experience varies by dose, timing, and injection site.
Some newer basal analogs extend even longer, aiming for smoother day-to-day control. Your selection depends on glycemic targets, daily routine, and your clinician’s judgment. For label summaries and safety highlights, see Lantus Insulin Uses for a practical overview of glargine’s role in basal therapy (Lantus Insulin Uses). You can also review the FDA-approved details in the product labeling (Lantus prescribing information).
Insulin Peak Times and Duration: Quick Reference
Use this brief insulin peak times chart as a starting point, then tailor it with your care team. Times are typical ranges, not guarantees, and may differ across people and doses.
| Type | Onset | Peak | Duration | Examples |
|---|---|---|---|---|
| Rapid-Acting | ~10–20 minutes | ~1 hour | 3–5 hours | Lispro, Aspart, Glulisine |
| Regular (Short-Acting) | ~30 minutes | 2–4 hours | 5–8 hours | Regular |
| Intermediate-Acting (NPH) | 1–2 hours | 4–12 hours | 14–24 hours | NPH |
| Long-Acting (Glargine/Detemir) | 1–2 hours | Minimal | Up to 24 hours | Glargine, Detemir |
| Ultra-Long (Degludec) | 1–2 hours | Minimal | >24 hours | Degludec |
These ranges come from label data and clinical summaries. For a deeper walk-through of each class and its use-cases, see Types of Insulin for context on matching treatments to needs (Types of Insulin). For formulation-specific information on fast analogs used at meals, see Novorapid Cartridge for brand examples and delivery format details (Novorapid Cartridge).
Practical Timing Strategies and Meal Planning
Matching meals to insulin action can lower variability. The short acting insulin peak of rapid analogs often occurs around one hour, so some people choose to dose shortly before eating. Others pre-bolus earlier when meals are high in carbohydrates or have a high glycemic index. Your plan should reflect your clinician’s guidance and your glucose patterns.
Consider digestion rate, fiber, fat, and protein. Activity within two hours after dosing may accelerate absorption and increase sensitivity. Keep glucose checks, sensors, or logs active around new routines. For a plain-language explainer on timing with fast analogs, see What Is Rapid-Acting Insulin for examples and planning tips (What Is Rapid-Acting Insulin). If you use pens, see Types of Insulin Pen to compare delivery choices and dose increments (Types of Insulin Pen).
Safety, Side Effects, and Hypoglycemia Risk
All insulins can cause low blood sugar. Known insulin lispro side effects include hypoglycemia, injection site reactions, and rare allergic responses. Rotating injection sites may reduce lipodystrophy (fat tissue changes). Review your sick-day plan and discuss hypo treatments with your clinician so you can act early if needed.
For label-based safety details and practical handling notes, see Humalog Vial Guide for sections on warnings and precautions (Humalog Vial Guide). For formulation specifications, concentrations, and handling, see Insulin Humalog Vial for product details that can inform safe storage and use (Insulin Humalog Vial). Broader safety context appears in American Diabetes Association guidance (insulin basics), which also outlines hypoglycemia prevention.
Related Reading and Tools
If you are exploring prandial options, comparing analogs can clarify fit. For a concise brand comparison, see Humalog vs. Novolog to understand similarities and differences in timing and formulation (Humalog vs. Novolog). For fundamentals of insulin therapy in autoimmune diabetes, see Type 1 Diabetes Insulin for care pathway context (Type 1 Diabetes Insulin).
Additional practical articles live in our diabetes library. For continuing education on technology, dosing devices, and lifestyle strategies, see Diabetes Articles to browse updates and explainers across topics (Diabetes Articles).
Recap
Insulin timing shapes daily control, safety, and confidence. Lispro acts fast, regular peaks later, NPH peaks broadly, and long-acting options provide steadier baselines. Use label ranges as guardrails, then personalize with your clinician. Keep logs, watch trends, and adjust routines cautiously.
Note: Peaks and durations are approximate. Illness, activity, stress, and site rotation can shift your experience. When in doubt, prioritize safety and verify with your care team.
This content is for informational purposes only and is not a substitute for professional medical advice.