If you think your blood sugar might be creeping up, learning the signs and symptoms of prediabetes can help you act early. Prediabetes means your glucose is higher than normal but not in the diabetes range. Doctors use tests like A1C (glycated hemoglobin) and fasting plasma glucose to confirm it. Early attention to nutrition, movement, sleep, and stress can delay or prevent type 2 diabetes.
Most people notice few or no clear warning signs. Subtle patterns—daytime fatigue, increased thirst, or frequent urination—can be easy to miss. That is why screening and risk awareness matter. The sooner you know, the more choices you keep.
Key Takeaways
- Subtle signals first: Energy dips and increased thirst may precede clear changes.
- Know your numbers: A1C, fasting glucose, and 2‑hour glucose guide decisions.
- Small steps add up: Balanced meals, daily movement, and better sleep help.
- Targeted follow-up: Repeat testing and risk-specific plans reduce progression.
Signs and Symptoms of Prediabetes
Prediabetes often develops quietly. You may feel more tired after meals or notice nighttime urination more than before. Some people have increased thirst, mild headaches, or blurry vision after large, carb-heavy meals. Skin changes can appear too, including acanthosis nigricans—velvety darkening on the neck, armpits, or knuckles—and small skin tags. These clues reflect insulin resistance (reduced insulin effectiveness) rather than full diabetes.
Women may experience irregular cycles or worsening symptoms in polycystic ovary syndrome, which overlaps with insulin resistance. Men might report increased waist circumference and early nerve tingling in the feet. Slow-healing scrapes, more frequent yeast infections, or dry, itchy skin can also show up. To compare overlapping features with later-stage disease, see Type 2 Diabetes Symptoms for a practical contrast discussion.
Who Should Get Tested and Why It Matters
Testing is important if you have excess weight, a family history of diabetes, a history of gestational diabetes, sleep apnea, or you belong to groups with higher risk. Age and abdominal fat raise risk further, as does polycystic ovary syndrome. Some people also report prediabetes symptoms like increased thirst and fatigue after large meals. Even when you feel fine, screening can prevent missed opportunities to act early.
Without changes to diet and activity, a significant portion of people progress to type 2 diabetes within a few years. Community-based programs and simple habit shifts reduce that risk. For step-by-step testing guidance and what each test shows, see How To Test For Diabetes. If you want a plain-language explainer of underlying biology, our overview What Is Insulin Resistance describes how insulin’s signaling gets disrupted over time. For those with cycle or fertility concerns, PCOS Symptoms explains the connection with insulin resistance.
According to the U.S. Centers for Disease Control and Prevention, structured lifestyle programs and weight loss can substantially reduce progression to diabetes in high-risk adults. See the CDC prediabetes overview for definitions and program fundamentals.
Understanding Your Numbers
Clinicians diagnose prediabetes using three standard tests. A1C estimates average glucose over about three months. Fasting plasma glucose checks morning levels after at least eight hours without calories. The oral glucose tolerance test measures how your body handles sugar over two hours. A simple normal blood sugar levels chart can help you remember the cutoffs. Keep in mind, slight differences may occur between labs.
| Test | Normal | Prediabetes | Diabetes |
|---|---|---|---|
| A1C (%) | Below 5.7 | 5.7–6.4 | 6.5 or higher |
| Fasting Plasma Glucose (mg/dL) | Below 100 | 100–125 | 126 or higher |
| 2‑Hour OGTT (mg/dL) | Below 140 | 140–199 | 200 or higher |
These targets come from major professional guidelines used in clinics. For formal criteria and testing recommendations, see the ADA diagnostic thresholds. If home monitoring interests you, check our later section on meters and practical next steps.
A1C, After-Meal Spikes, and Red Flags
People often ask what is a dangerous level of a1c. In clinical practice, an A1C at or above 6.5% meets diabetes criteria, but danger also depends on symptoms, other health issues, and how quickly numbers are rising. Sudden high readings with dehydration or confusion require urgent evaluation. Stable, modest elevations need follow-up and lifestyle support.
After-meal readings offer additional context. Two hours after eating, many clinicians look for values under roughly 140 mg/dL in people without diabetes. Temporary spikes can occur after larger or more refined-carb meals. Discuss your target range with your clinician, because individual goals differ by age, medications, pregnancy, and heart or kidney status. For a deeper look at the test itself, the NIDDK A1C test page explains how labs calculate this index.
Food, Movement, and Sleep: Daily Habits That Help
A practical prediabetes diet emphasizes non-starchy vegetables, lean proteins, healthy fats, and high-fiber carbs. The plate method works well: fill half the plate with vegetables, a quarter with protein, and a quarter with whole grains or starchy vegetables. Adding beans, lentils, nuts, and seeds helps tame post-meal spikes. People who plan meals ahead find it easier to stay consistent on busy days.
Movement boosts insulin sensitivity quickly. Try brisk walking, cycling, or swimming for 150 minutes each week, plus two strength sessions for muscle support. Sleep also matters; aim for seven to nine hours on a regular schedule. Manage stress through brief breathing drills or short walks. For broader context on where prediabetes sits among related conditions, see Types Of Diabetes for distinctions that guide prevention choices.
Tip: Prep a simple weekly menu to reduce last‑minute, high‑carb choices. If you use a meter, pair meals with short walks and review patterns. For those curious about self-checks, our section below covers home tools and practical targets.
Treatment Options and Follow-Up
First-line prediabetes treatment focuses on structured lifestyle support—nutrition coaching, activity plans, sleep hygiene, and stress reduction. Clinicians may also recommend weight-management programs or community classes. In select, higher-risk cases, a clinician may discuss metformin (a glucose-lowering biguanide) to reduce progression risk. This medication choice should weigh benefits, tolerability, and personal goals.
Follow a schedule for repeat testing, usually every three to twelve months depending on risk and earlier results. Keep eye on blood pressure and cholesterol too, because cardiometabolic risks travel together. To understand metformin basics and how it compares with a common branded option, see Glucophage Vs Metformin for general background. For more learning across prevention and care topics, browse our Type 2 Diabetes posts to find practical, stepwise strategies.
Individual Factors and Life Stages
Hormones, age, sleep, and medications all influence glucose. Pregnancy changes targets, and a history of gestational diabetes raises future risk. Women with polycystic ovary syndrome often experience stronger insulin resistance; addressing weight, sleep apnea, and activity can help. Men may see faster waist growth and earlier blood pressure changes. Tailor your plan to your stage of life and any overlapping conditions.
Some people ask how to interpret the prediabetes range a1c as they get older. The core cutoffs are similar, but personal targets may shift with frailty, heart disease, or kidney issues. Discuss goals that fit your health profile. If you suspect cycle-related changes or fertility concerns, revisit the link to PCOS Symptoms for a concise, hormone-focused overview that connects to metabolic health.
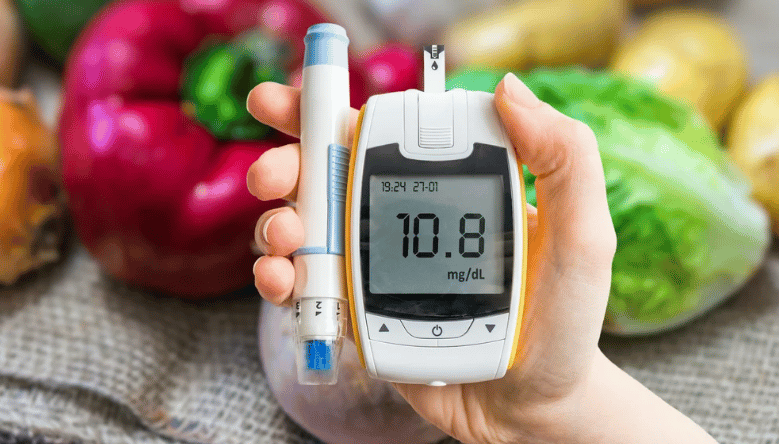
Monitoring at Home and When to Seek Care
Fingerstick meters and occasional post-meal checks can reveal useful patterns. Testing before and two hours after a few typical meals helps you see which foods fit your plan. For a helpful walkthrough on test choices and timing, visit How To Test For Diabetes to learn practical steps for home and lab use. If you prefer Bluetooth syncing and color-coded ranges, consider Onetouch Verio Flex Meter as an example of a meter that simplifies trend spotting.
Check feet weekly for cuts, blisters, or color changes, especially if you notice tingling or numbness. Skin care matters too—hydrate dry areas and watch for darkened patches around the neck or armpits. If you use a meter regularly, you may need fresh strips; see Onetouch Ultra Test Strips for a quick reminder about matching strips to your exact meter model. Seek prompt care for vision changes, chest pain, severe dehydration, or infection.
Recap
Prediabetes sits on a spectrum—your choices today can shift the path. Understand your numbers, shape meals around fiber and protein, and move most days. Prioritize sleep and keep stress manageable. These changes help insulin work better and keep glucose steady.
Partner with a clinician for testing and a plan that fits your life. Use community resources and simple tools to build momentum. For deeper background on related conditions and prevention, our links throughout this guide point to stepwise, practical reading.
Note: Thresholds and targets vary by condition, pregnancy status, and medications. Your clinician can personalize goals to your safety and priorities.
This content is for informational purposes only and is not a substitute for professional medical advice.